If you think you’re infected
Week 11 (March 9-15)
Do I have COVID?
The most tell-tale signs of a COVID infection are:
-Fever
-Dry cough
-Shortness of breath
More details on symptoms here.
A snuffy/runny nose is a sign that you probably have just a regular respiratory infection.
What do I do now?
If you are severely ill, go to the hospital. If you think you can rest at home, call your doctor. Your doctor will probably tell you just to stay home, hydrate, and self-isolate for 14 days. There are no treatments available at this time. This is a virus, not bacteria, so antibiotics are not helpful.
Should I try to get tested?
There are many advantages to knowing if you’re positive or negative for COVID. You can inform people you had prior contact with, since there does seem to be transmission in conjunction with the very first mild symptoms.
When you recover from COVID, you will have immunity for at least the near term. When all hell breaks loose, it would be highly useful to have a cadre of people who know they are immune who could be on the front lines to serve vital roles in the community. For example:
(a) Delivering groceries and essentials to older people at home
(b) Interacting with patients arriving for COVID testing at drive-through clinics
That said, there is a severe shortage of testing capacity for COVID. Most people are being told to not even try.
How Afraid Should I Be?
Week 11 (March 9-15)

There’s a simple reason people can’t decide whether they should be scared out of their wits or shrugging off COVID. It’s because human brains are not good at thinking at abstract population levels. Even doctors’ brains. But you cannot understand the current COVID situation if you don’t have a simple understanding of contact networks and population-level risk. So I’m going to give it a try:
Why you will be scared. COVID is frightening at a population level. At some point, in the upcoming year, someone you know personally is going to die of COVID.
This is because:
In a likely scenario, around 40% of the population will be infected. So if you know 1,000 people, 400 will get the virus.
Maybe half will show symptoms (200 people). Of those, 0.5-1% are estimated to die (1-2 people).
Social networks are complex and variable. You might not have 1,000 close friends, but if you have a couple hundred friends on Facebook, and know many of their friends and family members, plus people you went to school with, people your kids go to school with, and their parents….well, pretty soon your contact network starts to grow exponentially and a thousand is probably a pretty low-ball number.
Why you should not be panicked. The natural instinct is to panic when you hear about people you know getting severely ill and dying. But no matter what happens around you, you must remember that the circle of people you know is probably larger than you realize, and your personal risk is still very low if you are a young, healthy adult or child. Even if you get infected, you have a very slim chance of severe illness.
In the near term, what this means is that your decision to limit your social contacts over the next weeks and months is not so much for your personal health, or that of your children, but for your community and your circle of contacts, especially those at high risk.
That’s why it makes strong mathematical sense to upend your life in many ways, to protect your larger community, but not to panic, recognizing that your personal health is probably not at great risk.
Also, expect that there will absolutely be news reports about children and young people getting severely ill and dying. If large enough numbers of them get infected, there will inevitably be a small number that have poor outcomes. But these news reports do not change the fact that you are low risk.
Don’t Panic
Week 11 (March 9-15)
What a difference a night makes. Tom Hanks has COVID. The NBA and MLB canceled games. It’s going to suddenly become a whole lot easier for mayors to close schools and cancel senior bingo games. Most Americans now recognize that COVID is going to have a major impact on their daily lives. At this time, our goal is that no American city ever looks like Wuhan. Accomplishing that will require collective action and changes to how we socialize and work over a period of weeks or months. Certain economies will be hit very hard. But here are a couple thoughts to help you sleep at night:
- Our children are safe. For unknown reasons, children, teenagers, and young adults are not getting severely ill from COVID. During past influenza pandemics, deaths were concentrated in children and young adults. Young people with underlying conditions are still at risk. But it should help us all sleep better to know that most children do not appear to be at risk for severe disease.
- Tony Fauci. The director of the NIH infectious disease branch is possibly the most revered government official in the country. Serving since 1984, he has guided 5 US presidents on infectious disease threats — HIV/AIDS, SARS, Ebola. We are currently in a leadership vacuum. But having a high-level figure with impeccable scientific credibility who is deeply respected by both Republicans and Democrats in congress should help us sleep at night.
- Tom Hanks probably won’t die. We don’t know the precise fatality rate because our knowledge of mild cases is so low. But we do know that death rates get higher as you get older. At age 63, Hanks is in a higher risk group. The risk of death in the 60-69 age group is 3-4 fold higher than the 50-59 age group. But it’s still probably only a bit higher than 1 out of 100. Tom Hanks was already an American hero. But it’s possible that his decision to report his infection will save Americans lives by getting everyone to finally take this seriously.
Canceling big events
Week 11 (March 9-15)
Summary: COVID is more widespread than the numbers suggest. Waiting until you already have cases in your community before canceling large events will make your epidemic more intense and difficult to control. When you start flooding hospitals with sick people is when people really start dying.
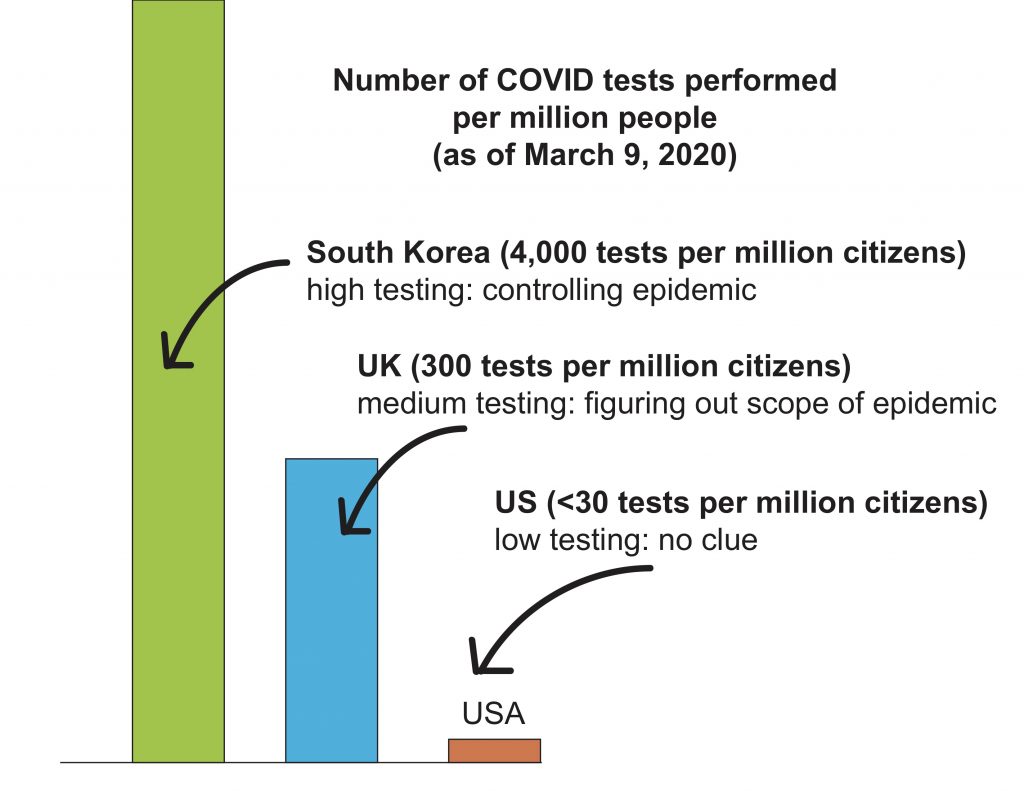
(a) ð–ðž ð¡ðšð¯ðž ð§ð¨ ðœð¥ð®ðž ð¡ð¨ð° ð¦ðšð§ð² ð€ð¦ðžð«ð¢ðœðšð§ð¬ ðšð«ðž ð¢ð§ðŸðžðœððžð ð°ð¢ðð¡ ð‚ðŽð•ðˆðƒ. We are still woefully behind in testing for COVID. As of March 9, the UK has tested 18,000 people more than the US (26k vs 8k). That’s 15x more at a population level (per million citizens). Of 18 countries, the only ones the US ranks ahead of in testing are Vietnam and Turkey. We are driving blind. Individuals can’t make decisions about holding or attending events. Local leaders can’t make decisions about canceling schools. At these testing rates, by the time the virus is detected in a community, it’s probably already widespread and will be very difficult to stop.
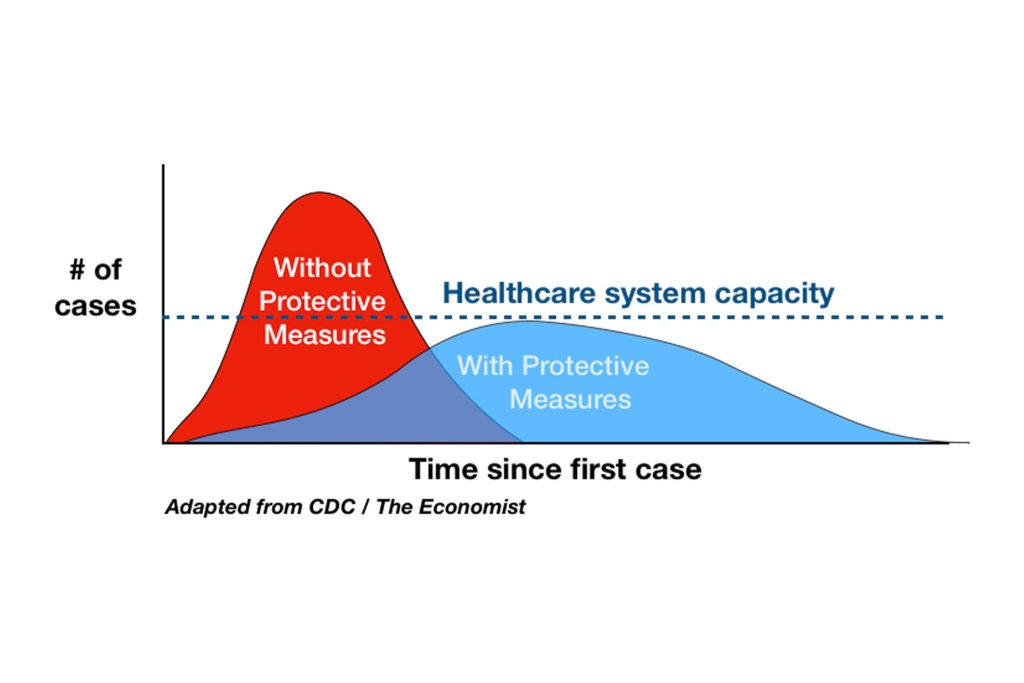
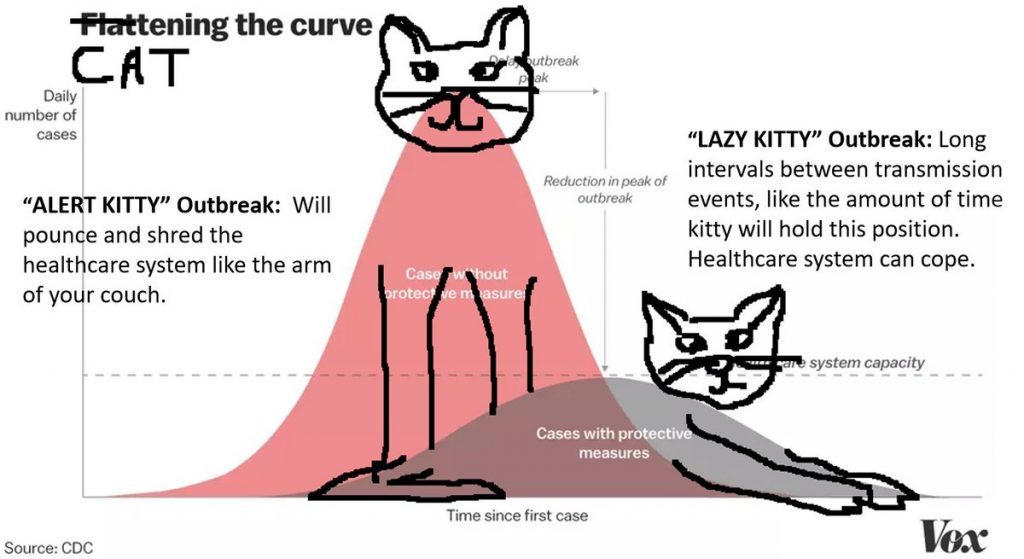
(b) ð…ð¥ðšðððžð§ ðð¡ðž ðœð®ð«ð¯ðž. We’re not going to be able to stop COVID from transmitting. And if you start to run the numbers (say, 40% attack rate, and 10-20% hospitalized) and take inventory of the number of hospital beds, respirators, PPE in your state or community, you pretty quickly realize that we don’t have anywhere near the capacity for a full-blown COVID epidemic. Especially if healthcare workers are getting sick themselves.
Either act too early, or too late. Aggressive social distancing measures, even before there are confirmed cases, can slow the progression of the epidemic before it takes off. Americans are not particularly socialist by nature, but this is a case where individual sacrifices can collectively dampen the spike of an epidemic and save lives. Again, healthy people don’t need to seal themselves in their house. But be prepared for the cancelation of large events — concerts, sports events, political rallies, etc. I’ve been so impressed by the social consciousness of friends and family and the willingness to alter behavior, cancel plans, and think of the less fortunate. When local leaders and businesses start making very difficult decisions to cancel events, think about the 52 million Americans over age 65 and 133 million Americans with a chronic condition, and maybe resist the temptation to criticize. By the end of this, most of us will know someone who died of COVID, and in retrospect the sacrifices will seem small.
Credit: Anne Marie Darling @amdar1ing
Protect Granny

Week 10 (March 2-8)
It’s been a week since my post about COVID-19. Here’s the latest.
ð‘¹ð’Šð’”𒌠ð’ˆð’“ð’ð’–ð’‘ð’”
If you’re in a risk group (e.g., elderly*, underlying conditions), the time to think about social distancing has come. The virus is now transmitting in US communities. It may not be in your community yet. But we don’t know. You don’t have to seal yourself in your home, but you may want to avoid large gatherings. Try to be reasonable. Book club: probably okay. Going to a conference with 10,000 people and shaking everyone’s hand: probably less okay.
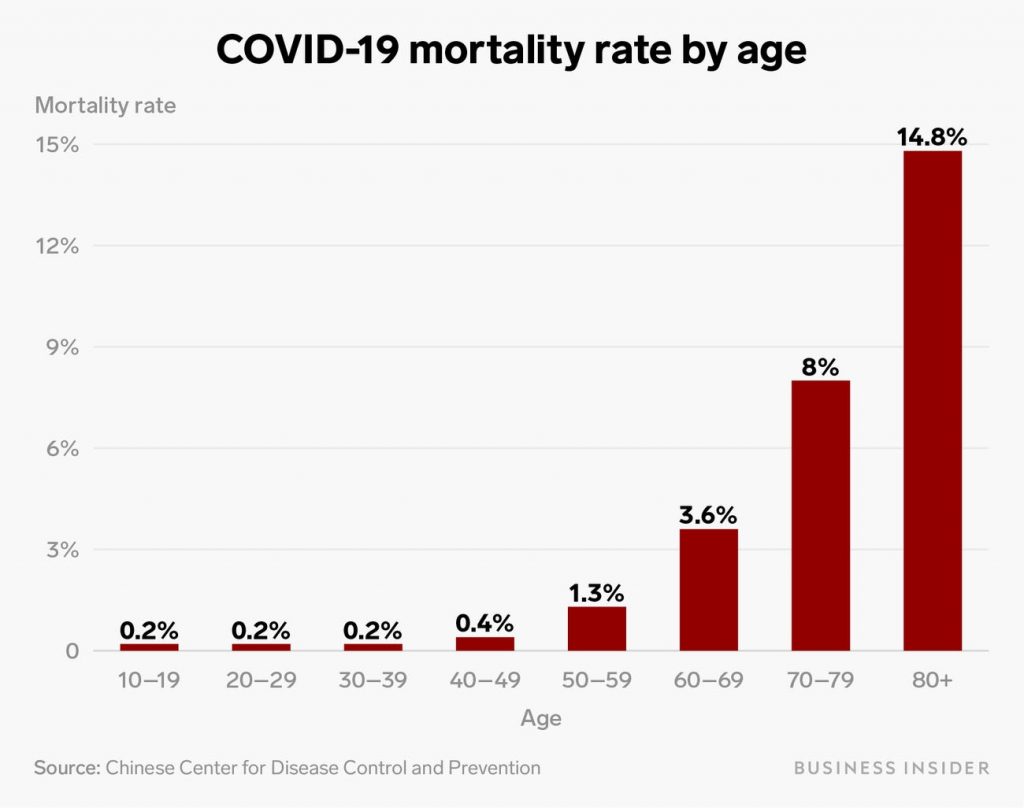
The exact numbers may not be correct due to underreporting of mild cases.
ð‘µð’ð’-ð’“ð’Šð’”𒌠ð’ˆð’“ð’ð’–ð’‘ð’”, ð’˜ð’Šð’•ð’‰ ð’“ð’Šð’”𒌠ð’ˆð’“ð’ð’–ð’‘ ð’„ð’ð’ð’•ð’‚ð’„ð’•
If you’re not in a risk group, you have less risk of severe disease. But if you get infected and have mild or no illness, you could still transmit the virus to someone in a risk group. So if you have high contact with people in a risk group, you may want to consider a degree of social distancing yourself. Again, being reasonable. Taking the dog to the park: okay. Taking a cruise: less okay.
I wish I could provide an app where you put in your age/health history and you could submit various activities (grocery shopping, Caps game, flight to Florida, attend granddaughter’s nursery school class) and the app would tell you the level of risk. Honestly, the data is just not there yet. We still don’t know, for example, how important children are in community transmission. You just have to try to use common sense and protect the vulnerable.
ð‘ð’–ð’•ð’–ð’“ð’† ð’‘ð’“ð’ð’”ð’‘ð’†ð’„ð’•ð’”
If the United States was China, I’d be confident that we could avert a major epidemic. China has effectively beaten back the virus without any vaccine or any special treatments. If you put society on lockdown, and practice extreme social distancing, you can break transmission and cases will drop, saving thousands, potentially millions, of lives. Italians have learned this lesson the hard way and have now initiated extreme lockdown of 16 million people. You know Italy is taking a virus seriously when they cancel the football games.
But we are not the Chinese. Or the Italians. We are the land of Don’t Tread on Me bumper stickers. And we are in an election year where politics come into play. Brace for a new meaning for March Madness.
*I intentionally use a vague term like ‘elderly’ because a fit 70-year old may be less risk than a frail 60-year old.
Be Prepared
Week 9 (Feb 24 – Mar 1)
I’ve been fielding a lot of questions about COVID-19 lately. Here’s a summary from your friendly neighborhood epidemiologist:
1. ð˜ðžð¬, ðð¡ðž ðœð¨ð«ð¨ð§ðšð¯ð¢ð«ð®ð¬ ð¢ð¬ ð©ð«ð¨ð›ðšð›ð¥ð² ðœð¨ð¦ð¢ð§ð ðð¨ ðš ðð¡ðžðšððžð« ð§ðžðšð« ð²ð¨ð®. The testing criteria has been so restricted in the US, we’ve likely missed dozens of mild cases that were imported weeks ago. A vaccine will not be available for at least a year. Exactly when the virus will hit your community depends on a lot of factors, but it could be sooner than you think, so good to be prepared and informed.
2. ð’ð¡ð¨ð®ð¥ð ðˆ ð›ðž ðŸð«ðžðšð¤ð¢ð§ð ð¨ð®ð? At this precise point in time, an American is more likely to die of seasonal influenza than COVID. But that could change dramatically if COVID starts transmitting through the US population. COVID is far more deadly than seasonal flu, even accounting for uncertainty in the fatality rate.
The risk for severe disease follows a ð’”ð’•ð’“ð’ð’ð’ˆ ð’‚ð’ˆð’† ð’ˆð’“ð’‚ð’…ð’Šð’†ð’ð’•, with most deaths in those over 70. That said, substantial mortality has also been observed in people in their 50s and 60s. And the millions of younger adults with chronic conditions (e.g., COPD, diabetes, hypertension) are also at risk. Testing has so far been so limited to severe cases so it’s hard to know what the denominator of mild cases is. But even a 1-2% fatality rate is extremely high [as context, Spanish influenza killed 20-50 million globally and had ~2% fatality rate in 1918}.
But the best news so far is that young children seem to be getting spared.
3. ðˆð’ð¬ ð§ð¨ð ðð¨ð¨ ðžðšð«ð¥ð² ðð¨ ðšð¬ð¤ ð²ð¨ð®ð«ð¬ðžð¥ðŸ: ðð¨ ðˆ ð¡ðšð¯ðž ðð¡ðž ð¬ð®ð©ð©ð¥ð¢ðžð¬ ðð¨ ð¬ð¡ðžð¥ððžð« ð¢ð§ ð©ð¥ðšðœðž ðŸð¨ð« ð°ðžðžð¤ð¬ ð¨ð« ð¦ð¨ð«ðž, ð¢ðŸ ð§ðžðžððžð. If you get infected and don’t require hospitalization, you may need to be self-quarantined in your own home for several weeks. Self-quarantine may also be an option for those at high risk when the epidemic is peaking in your community. Especially for retirees, teleworkers with existing health problems, you should think what degree of social distancing you can reasonably achieve. Between now and then, it would be good to think about stocking up on vital medications and essential supplies so you can minimize time in the community. It’s hard to know exactly how long a virus will be widespread in a given area. It’s a lot of complicated math that takes into account the characteristics of how the virus transmits and the demography and movement patterns of the community. It could be weeks, it could be months.
4. ð–ð¢ð¥ð¥ ð¬ðœð¡ð¨ð¨ð¥ð¬ ðœð¥ð¨ð¬ðž? Japan’s recent decision to close schools is not because kids are at risk for severe disease, but more because the country is under enormous pressure from the 2020 Olympics and it’s not clear if kids with mild infections are important in community transmission. It doesn’t look like children are driving community transmission, but government officials at all levels will be under extreme pressure to show they’re doing something, and without a vaccine or therapeutics, school closings may be all they have.
5. Q&A section:
– ð‚ðšð§ ðˆ ðžðšð ðšð ð‚ð¡ð¢ð§ðžð¬ðž ð«ðžð¬ððšð®ð«ðšð§ðð¬?
YES!
– ð’ð¡ð¨ð®ð¥ð ðˆ ð›ð®ð² ðš ð¦ðšð¬ð¤?
Most masks only protect against large respiratory droplets, not the fine aerosols that transmit viruses. Masks tend to be most useful when worn by someone who is already infected to prevent infection to others.
– ð–ð¨ð§’ð ðð¡ð¢ð¬ ðšð¥ð¥ ðð¢ðž ð¨ð®ð ð¢ð§ ð€ð©ð«ð¢ð¥ ð°ð¡ðžð§ ðð¡ðž ðœð¨ð¥ð ð¬ðžðšð¬ð¨ð§ ð¢ð¬ ð¨ð¯ðžð«? Pandemics don’t follow typical seasonality. Recall that the 2009 ‘swine flu’ pandemic started in April and the first wave went through June. Even if coronaviruses are typically winter pathogens, when there are so many susceptible people in a community with no immunity to a novel pathogen, it can transmit fine outside their regular season.
– ð–ð¡ðšð ðšð«ðž ðð¡ðž ðð¡ð¢ð§ð ð¬ ðˆ’ð¦ ð©ðžð«ð¬ð¨ð§ðšð¥ð¥ð² ð¦ð¨ð¬ð ðœð¨ð§ðœðžð«ð§ðžð ðšð›ð¨ð®ð?
* The low availability of tests in the US.
* Health systems that lack the protective equipment, beds, tests, etc. needed to protect their workers on the front lines and serve their community during the peak of the epidemic.
* Politicization of the outbreak. The 1918 Spanish flu was one of the worst disease events in history, killing 20-50 million people, more than all world wars combined, and it was so bad because during the war politicians didn’t want to hurt morale and hid the details, exposing millions of people. They actually held huge war parades in cities in the middle of the epidemic. The best way to fuel an epidemic is to put politics ahead of transparency and information.
