A Marmot’s Survival Guide for the Fall of 2020 (i.e., it’s better to know if we’re screwed and plan for it)
Dear America,
By now, six months into the COVID pandemic, you’re probably ready to punch someone in the face. Maybe you lost your job. Maybe your local school district just told you they’re not offering in-person school this fall. What the bleep am I going to do with my children?? Maybe you’d like to sucker punch one those guys who still won’t wear masks at the grocery store. Or young people taking selfies at bars. Or just Floridians in general.
But this is not where your anger should be directed. Many people aren’t helping the COVID situation. But they’re not the crux of the problem. You know what you should really be angry about? Testing.
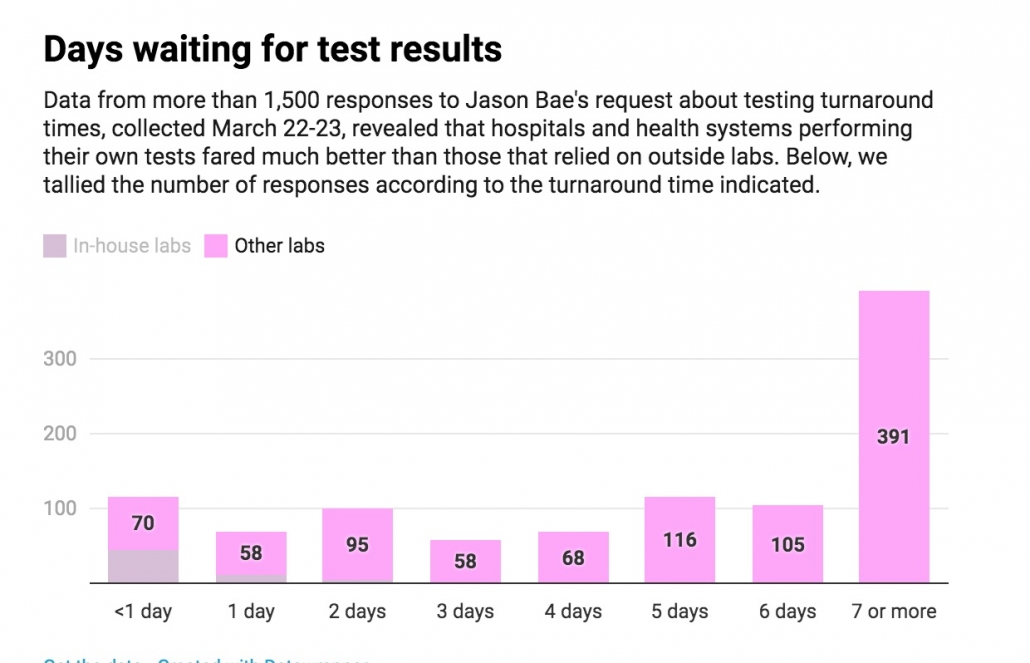
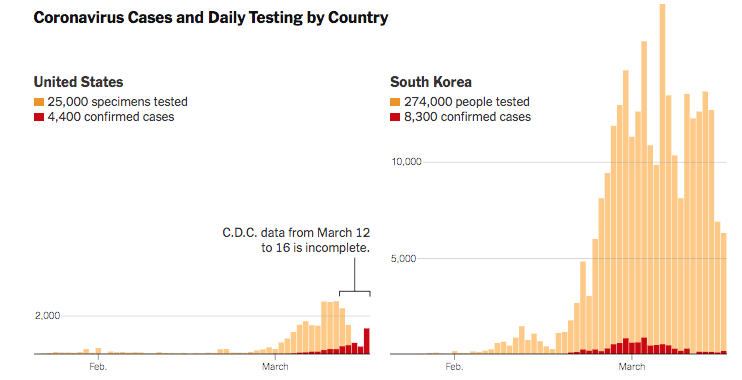
America’s testing capacity has greatly expanded since March. America currently produces more tests than any other country. We even have fun saliva tests you can ship from your home directly to the lab. But the volume of tests is not the most important measure of success. It’s speed.
Atlanta Mayor Keisha Lance Bottoms was recently a victim of America’s Great Testing Failure. Bottoms had her entire family tested for COVID on June 29 as a precaution after attending the funeral for Rayshard Brooks, a 27-year-old African American man who was fatally shot by Atlanta Police Department (APD) officer Garrett Rolfe.
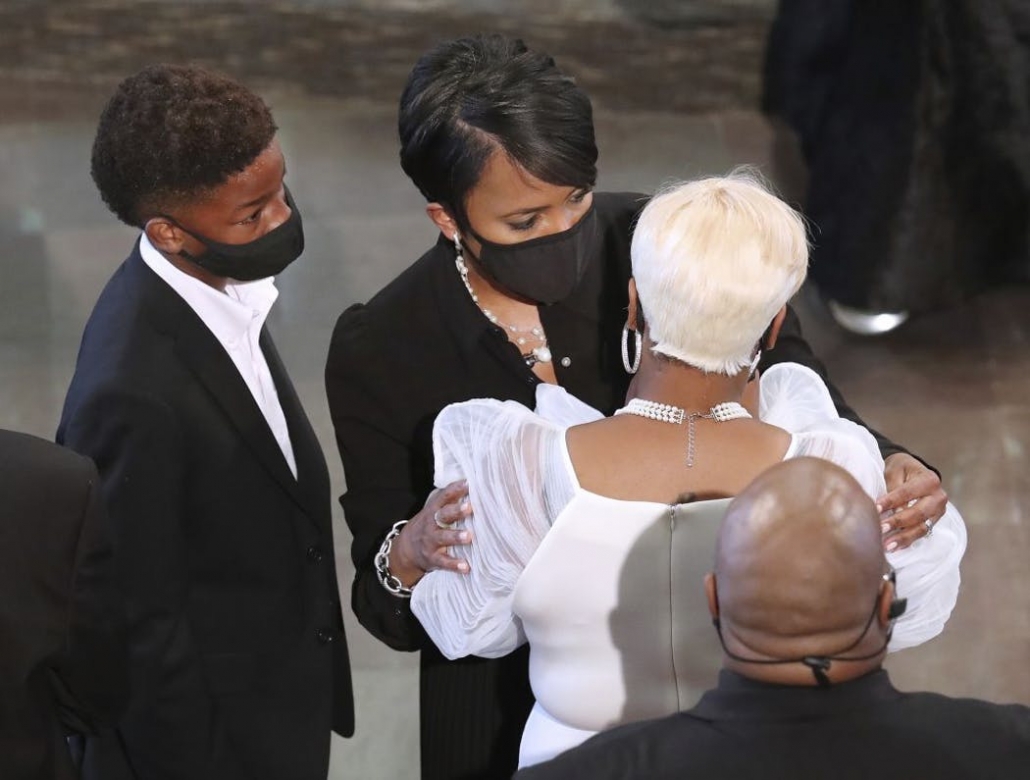
A week later her test results still hadn’t come back. With her husband starting to feel ill the family went to Emory University to get a different rapid test. Within hours, Bottoms learned that she, her husband and one of her four children were positive.
The results from the initial test finally arrived the next day (8 days after the swabs were sent). They showed that when the family first got tested, only one child was positive. Either Bottoms and her husband had gotten false-negative results, which is possible if the funeral had been the source of the virus and the Bottoms family was tested too soon after exposure, when false-negatives are common. Or the child had possibly passed it to his parents while they waited for their test results.
Either way, this example shows how long delays in test results help spread COVID. During the week when Mayor Bottoms was waiting for her results she didn’t have any symptoms. So she followed a normal mayoral routine, including holding a press conference and meeting with staff, potentially infecting other people.
It’s also worth noting that even the mayor of one of America’s largest cities had difficulty figuring out how to get a quick test in America’s tangled network of private and public laboratories. FDA has authorized rapid tests that can give a COVID result in hours. But first you have to find a place that has them. And maybe pay out of pocket. Vault’s at-home saliva test costs $150. And even if you can find a test that produces a result quickly, you’re in the dark about whether that test performs well or gives high rates of false results.
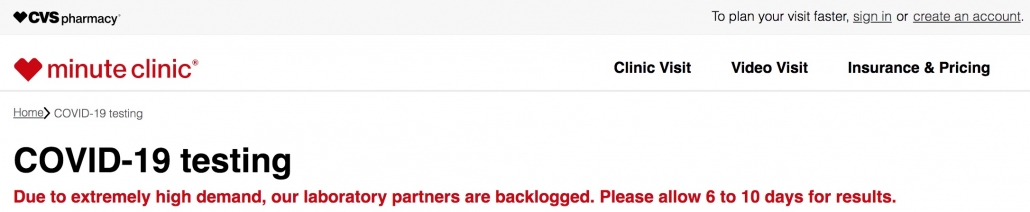
Ultimately, the longer the delays in test results, the longer asymptomatic people will be floating through society infecting other people. Which, by the way, happens to lead to more sick people, heavier demand on already stretched testing capacities, and, that’s right, even longer delays in testing. Welcome to the wonderful COVID Feedback Loop of Death!

The problem is that testing is only worthwhile if it is actionable. Test, trace, isolate does work in other countries like South Korea where you get a test result back in a day. When someone in a family tests positive (a) that person is isolated from other family members to reduce household transmission, (b) the family as a unit stays home to minimize the risk of infecting others in the community, (c) other family members immediately get tested, and (d) other friends or coworkers that the index case may have had contact with get immediately informed so they can get tested and isolate until they get the test result back to protect their own family. None of those actions to stop COVID spread happen if it takes a week to get a result back.
You can see how an American society that takes 8+ days to get test results back either (a) grinds to halt economically because staff and business can’t go back to work until test results come back or (b) spreads a lot of COVID around because asymptomatically infected people won’t know they’re positive until they’ve already spent a week infecting other people. The longer it takes for test results to get back, the higher the risk of asymptomatic people spreading COVID to their families and the community.
My overall point is this: we are asking Americans to battle COVID with everything they got: masks, social distancing, isolation. But we are not giving them a fighting chance if we don’t have rapid testing available. We are not giving schools a fighting chance. Or daycares. Or restaurants. Or even MLB.
Americans are determined to get back to business this fall. To open colleges, go back to the office, send kids off to school, even have some NFL games. We’ve been told to just write plans. Major League Baseball’s COVID plan alone runs 101 pages. My son’s preschool’s plan includes a schedule of when three-year old classes can use their designated bathroom. Dammit Jimmy you’re going to have to hold it until 3pm. Right now is the grasshoppers’ shift. Anyone who’s not impressed by the grueling effort to develop COVID plans and the sheer commitment of staff to perform the impossible should see how far they get trying to get a two-year old to hold their bladder for more than ten minutes.
But we’ve already seen glimpses of how quickly plans derail when even a single positive case occurs within a poorly functioning COVID testing infrastructure. This is not complex math. A lot of COVID in the community + of lot of asymptomatic carriers means an organization is likely to experience sporadic positive cases. Most of these cases will be isolated and not spread to others in the organization. But the operation is paralyzed until test results come back for all the COVID case’s contacts. The longer the wait for the test results, the longer the other employees/staff/students are stranded at home in limbo. With test results taking up to 8 or more days to come back, you can imagine it doesn’t take a whole lot of cases before people are spending as much time waiting at home as on site. You can get around this to some degree by siloing groups and limiting contacts and the number of people that need to quarantine (hence the miraculous rotational bathroom schedule at my son’s preschool). But many buildings are simply not constructed in a way in which groups will never share space. Especially when you include the ventilation system.
So while we’ve laid the burden of planning for COVID squarely on individual businesses and local governments, someone should start the waving the white flag around and point out that all these plans are useless if there’s no larger plan to make testing available for those that need it and to shorten the turnaround time between test and result. Just a couple weeks in, even the MLB practice schedule has been derailed by testing delays.
It’s not entirely clear why there is no national plan to develop testing capacity. A dire need for more testing happens to be the only thing economists and epidemiologists can actually agree on. Testing helps open the economy and keep people safe. It should be a bipartisan slam dunk.
We even have the nifty Defense Production Act (DPA) that can be wielded to get American companies to direct their resources towards producing materials critical to national security. Reagents and testing materials would certainly qualify.
But we don’t just need a plan for how to make more tests. We need a plan for how to shorten the turnaround time and deliver results quicker. To get tests to areas with critical shortages. We need a defined pipeline of new rapid test development, similar to what we have for vaccines and therapeutics. And we need reliable tests. Dozens of different tests have been granted Emergency Use Authorizations (EUA) by FDA. Including an in-home saliva test you ship directly to a lab that promises 48-72 hour results. But EUAs are evaluated on a rolling basis of submitted data and many could turn out to be unreliable. It’s tough to tell a 60-year old teacher to risk their life by showing up to class every day if students with suspected COVID cases can’t get a test result back in within a day or so. Or if a negative result has a high probability of actually being positive.
We also need to recognize that even with the DPA tests are not an unlimited resource. I know baseball is important, but there are 750 players plus a large entourage of managers, medics and staff that are being tested every other day. While ordinary Americans sit in hours-long waits. I’m not saying baseball isn’t worth it. I’m just saying that people in a positions of power should be debating this and not leave questions of access to whoever has the deepest pockets.
Pooling tests sounds like a simple way to improve efficiency. But that approach only works efficiently at lower levels of COVID positivity.
How hard would it be to develop a national plan for COVID testing? Well, a simple start would be to reappoint someone as the national testing czar, a position that was disbanded during earlier this summer. Remember that honeymoon period in May when everyone thought COVID had been kicked? Someone didn’t get the memo that the honeymoon is over.
But testing is an enormous logistical challenge that is beyond the capacity of any single czar. I certainly don’t fancy that improving testing is easy. But we haven’t really tried. We don’t have a testing task force. Or clearly stated goals. For not just the quantity of tests, but turnaround time, a robust pipeline of new tests in development, and rapid analysis of data to quickly determine which tests are crap and should be pulled from the market and which have promise and should be scaled up in production. Poor FDA was overstretched and underfunded even before COVID. And expect testing capacity to become even more strained in autumn and winter when cold and flu seasons begin and doctors need to distinguish COVID from other suspected respiratory virus infections.
Ultimately, what does it mean that we have no national testing plan? It means that all those plans written for schools and businesses are in a tight spot. Their success clings to the hope that COVID levels are so low in the community that they won’t have to deal with many positive cases. Maybe in Vermont. Not in Miami.
And in the end that means that a lot of places in America are going to need to brace for a rough fall. Because their plans have deep vulnerabilities that have nothing to do with a teacher’s ability to enforce pediatric bladder control. If you live in a place where COVID is still circulating uncontrolled in the community it is not too soon to start thinking about contingency plans for when schools close. Or daycares shutter. Or flights cancel. Or universities send kids home. Won’t it be fun to relive all those fun nostalgic memories from March 2020? Although six months into the pandemic it will be less scary and more infuriating. Because we had so much runway to get our act together. And just totally dropped the ball on the single most important thing.
Given this reality, how can a practical person try to prepare? First, if you’re a parent living in a state with rising COVID cases and low testing capacity, you should consider the real possibility that in-person schooling will shut down again this fall. Some large school districts have already announced that they’re not offering in-person education this fall. I have no perfect solutions for America’s impending wave of societal upheaval. But here’s my best advice: band together. Young children aren’t going to obediently follow online education for six hours a day. And parents need to get some work done. Consider creating pods of 2-3 families that are well-matched in the ages of their children that can have a rotation of designated parents across the week to supervise a mix of in-person and online learning.
Sure, this introduces a level of COVID risk. It’s accepting another family or two into your circle of trust. And it could be hard to find a family that is matched in terms of kids’ ability to sit still plus parents’ ability to supervise learning. Not to mention finding a family with similar thinking about masks, hygiene, etc. But we need to craft new systems and makeshift markets. Try outdoor education to minimize COVID risk. Maybe one parent focuses on music, another on outdoor play, another on history. Maybe one parent ends up doing more supervision than others and gets compensated financially for their time. We’re in the middle of a global catastrophe, so try to be flexible and keep the expectations low. A round of Haagen-dazs if the kids happen to learn anything.
TL;DR: America has made more COVID tests than any other country. But until we cut down the time it takes to get a test result our plans for opening schools, offices, and even baseball are threatened.
Primer on COVID Testing
PCR (virus detection): For people who think they have an active infection. Tests for virus genetic material in nasal passages or saliva. Highly specific (low rate of false positives). But potential for false-negatives, particularly for samples collected too soon after a person is exposed. [Note that virus genetic material can sometimes be detected by PCR long after a person is no longer infectious.]
Serology (antibody detection): For people who may have been infected in the past but were unable to obtain a test. Tests for antibodies in blood (i.e., immune responses specific to COVID infection). Variable performance makes serology useful for estimating the proportion of people in a population that have been exposed to COVID, but unreliable as a diagnostic test for individuals.
Antigen (virus detection): For people who think they have an active infection. Detects viral proteins in saliva or tissue swabbed from the nasal cavity. Cheap, fast, but considered unreliable. Only one antigen test so far has a EUA.
False Negative: A test that incorrectly gives a negative result for a person infected with COVID.
False Positive: A test that incorrectly gives a positive result for a person who is not infected with COVID.
Sensitivity: Proportion of test results that are false negatives.
Specificity: Proportion of test results that are false positives.
Positive Predictive Value: Probability that a positive test result correctly reflects that a patient has COVID-19. Depends on the performance specifications of a test (sensitivity and specificity) and how widespread the disease is in a community — a situation that can change rapidly.
Further reading:
Why some Covid-19 tests in the US take more than a week, MIT Technology Review
Individual EUAs for Molecular Diagnostic Tests for SARS-CoV-2
COVID 19 Testing – Guide for Physicians
Coronavirus antigen tests: quick and cheap, but too often wrong? Science

Leave a Reply
Want to join the discussion?Feel free to contribute!