The Marmot’s Guide to Life in COVID
In my last post I mentioned that people shouldn’t assess COVID risk solely based on the presence or absence of masks. But I didn’t clarify what criteria should be used instead. This is the order in which I generally evaluate COVID risk associated with a particular activity. This list is different from the more popular lists that assign individual activities a 1-10 risk level. Those lists are helpful in giving people a general sense of what kind of activities are higher risk. But the risk of going to a public swimming pool depends on how it’s operated. Are they limiting how many people can be in the pool or a lane at a given time? Are they opening indoor changing facilities? Is the pool located in a community with high COVID activity or low COVID activity? The devil is in the details. A conceptual framework might be more helpful. Here are 8 metrics to use, ranked from most important to least important.
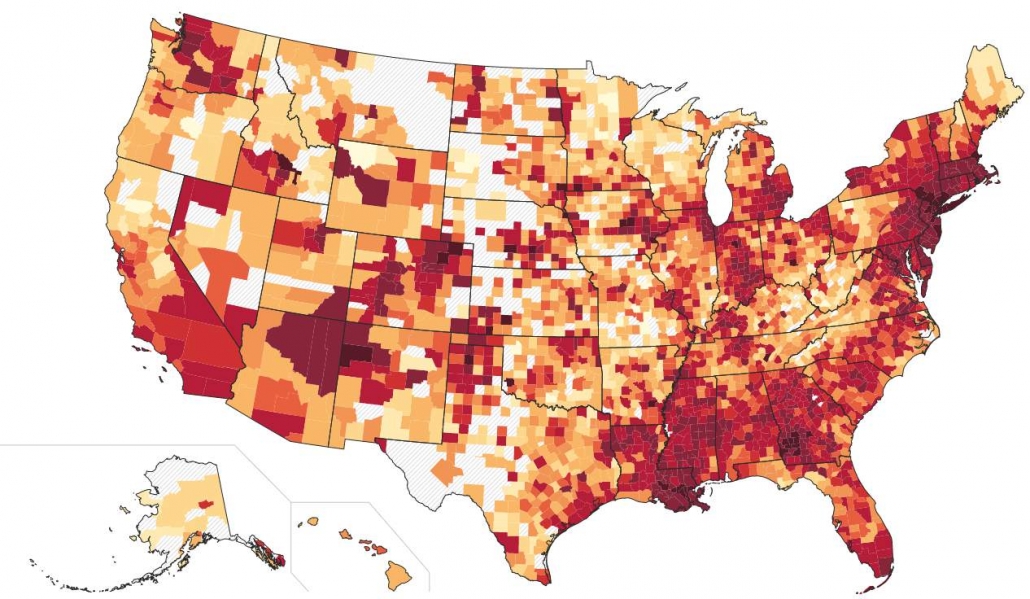
- Community Transmission. This is an obvious one. A pilates class in a COVID hot zone (currently Arizona) does not have the same risk as the exact same pilates class in a COVID cool zone (e.g., Vermont). This is a useful site for tracking COVID trends by state. Here’s a nice map for exploring by county. You can also check your state/city/county health department website for more local trends. How much COVID is circulating in a given place and time really matters and should be a top factor for evaluating risk. Stay informed.
2. Human Density. I recently had someone ask me if they should get on a plane if people weren’t wearing masks. I asked how full the plane was. How many empty seats? I would rather be on plane with lots of empty seats and no masks than a plane full of people wearing masks. And people should remember: six feet is a general guideline, not a magical number. [For a nice story on where the six feet rule originally came from, check out RadioLab].
3. Time Duration. COVID transmission is more likely to happen during sustained contact, not fleeting encounters. A 10 second encounter is different from a 5 minute encounter which is different from a 1 hour encounter. Time matters.
4. Indoor/Outdoor. COVID transmission is much more likely to occur in indoor settings than outdoor. Figuring out creative ways to move more activities outdoors should be a major component of any reopening strategy during COVID.
5. Invisible Contact Networks. This is a tricky one. But it’s really important. If you want to get your hair cut in a salon you can’t just think about what you see: the space, the number of people in the room, whether your stylist is wearing a mask or not. You have to think about you don’t see. The probability of your stylist carrying COVID depends on her invisible contact network. How many haircuts has she done this day/week? What are the contact networks of her contacts? It makes a difference if the stylist’s partner is working from home or on the front lines without PPE. What does your stylist do when she’s not cutting hair? These are much more difficult to ascertain. But when your safety is on the line, it is not crazy to need information that would otherwise seem like invasions of privacy.
6. Mucosal Ballistics. COVID transmission is enhanced by singing and loud talking particularly in enclosed spaces. Potentially exercising in enclosed spaces as well. Much of this is anecdotal, but there do seem to be superspreading events associated with choirs or work in buildings with extremely loud machinery that requires shouting for communication (e.g., meatpacking plants).
7. Ventilation Systems. Again, this one is less obvious. But airflows are important and will be a major consideration when we start thinking about bringing people make into enclosed spaces — gyms, schools, offices. Societally, there has been a big emphasis on buildings with climate control. We need a lot more research in this area. But some things are obvious, like opening windows and doors and improving circulation. This is not my particular wheelhouse at all, but it is something I do try to consider when running COVID-risk algorithms in my head. And it will need to be part of any long-term COVID reopening strategy.
8. Masks. Masks deserve to be on this list. But I have to admit that I can’t think of an example where I couldn’t make up my mind based on metrics #1-7. The presence or absence of masks has never tipped the scales.
TL;DR: Masks provide a strong visual cue that people around you take COVID seriously, providing a sense of safety. However, it takes a lot more than masks for an environment to be safe, including less visible factors like contact networks, community transmission levels, and air flows that should be strongly considered.

Much thanks for zip code information!
I wonder about restaurants that are serving outside? Is the risk there greater than getting a carry out?
It’s all about the duration of human contact, so delivery is less risk than eating at a restaurant outside. That said, eating at a restaurant outside is better than inside. Who you eat with and how well socially distanced you are from other customers also matters. And how well socially distanced the restaurant staff are from each other and from customers also matters.